Photo Credit: Internet
Clear Cut Health Desk
New Delhi, UPDATED: Sep 17, 2025 12:35 IST
Written By: Antara Mrinal
India is facing an emerging public health crisis in the form of drug resistant infections, making treatable diseases even more difficult, and in many cases, deadly. During the 15th Annual Conference of the Clinical Infectious Disease Society (CIDSCON 2025) from 11th – 15th September, 2025, recognized leaders in infectious disease raised alarms that almost 300,000 deaths per year in India can now be attributed to these infections. Over-prescription of antibiotics, poor diagnostic practices, and low public understanding around antimicrobial resistance (AMR), were all identified as contributing factors.
Further evidence is aligned with the Global Burden of Disease / Health Data estimations conducted by the Institute for Health Metrics and Evaluation (IHME), suggesting that in 2021 India faced approximately 267,000 deaths (with uncertainty interval 224,000–310,000) directly attributed to AMR and almost 987,000 deaths attributed to AMR (AMR contributed partly to the death although it was not the primary cause).
Who’s Raising the Alarm & What They Say#
Physicians speaking at CIDSCON 2025, such as Dr. V. Ramasubramanian (Chennai), are now voicing a sense of urgency about the need for students to receive some form of infection control education related to antibiotic misuse during their medical school training. Dr. Kamini Walia (Indian Council of Medical Research – ICMR) pointed out that the reason so many physicians resort to antibiotics as their default therapy is most often because diagnostics are not accessible over time, are too expensive, or not available.

Dr. V. Ramasubramaniyan and Dr. Kamini Walia | Photo Credit : Internet
Until better diagnostic structures are in place, antibiotics will continue to be over-utilized. Clinicians, such as Dr. Vasant Nagvekar (Lilavati Hospital, Mumbai), spoke about how treating tropical diseases like dengue, malaria, and leptospirosis is getting more difficult, due to drug resistance. Infectious disease specialists, such as Dr. Rajeev Soman, urged more policy measures.

Dr. Vasant Nagvekar and Dr. Rajeev Soman | Photo Credit : Internet
International organizations are also entering the conversation. The Global Antibiotic Research & Development Partnership (GARDP) has undertaken new analysis revealing significant voids in treatment for highly resistant Gram-negative bacterial infections in India and other low- and middle-income countries (GARDP report). An additional, critical voice belongs to the one health trust, which conducts AMR surveillance, policy briefs, and modelling, and has made it more explicit in its work which emphasizes how human health, animal health, environmental health, and antibiotic use in agriculture all fit under AMR, making the issue more difficult.
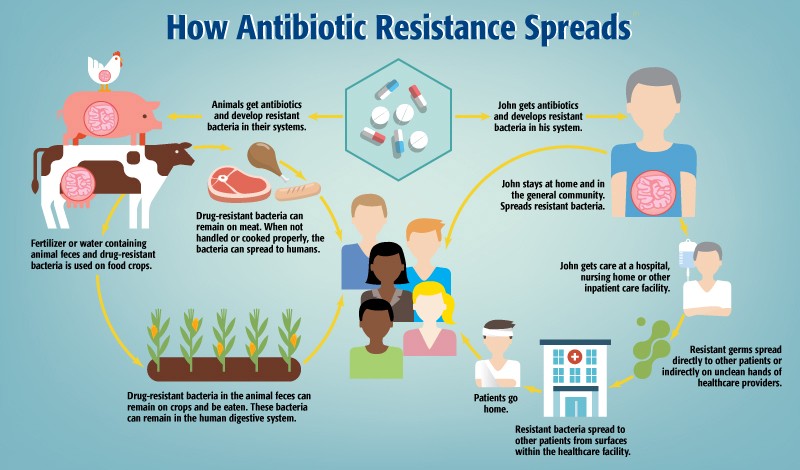
Photo Credit: Compass by Rau’s IAS
Why the Crisis is Escalating#
India’s AMR challenge arises from a combination of factors which are mutually reinforcing and make AMR a complex phenomenon that evolves over time. While there are many reasons contributing to AMR, the main factor is the overuse and misuse of antibiotics. The lack of reliable diagnostics means that many prescriptions are made without a credible diagnosis. Unjustifiably cheap broad-spectrum first-line antibiotics are often given and are perpetuating the avoidance of antimicrobial resistance. Compounded by significant deficiencies in diagnostic infrastructure, many clinics cannot provide reliable and immediate testing results. In the absence of useful tests, physicians are forced to rely on empirical treatments rather than acting on the careful assessments involved in targeted therapies. Elevated public and clinician cognizance which contribute to AMR is yet another compounding factor. The lack of understanding of what antibiotic stewardship means, which is, using antibiotics only when necessary, and according to guidelines, is problematic. Finally, undertreatment and access issues mean that even when effective drugs do exist they are not even prescribed or accessible to patients. A Global Antibiotic Research and Development Partnership (GARDP) study reported that the majority of people in India with highly drug-resistant infections never received the appropriate antibiotic, while only a minority received the correct antibiotic. Taken together, these gaps make AMR undoubtedly one of the most urgent multifaceted public health problems facing the country.
A recent “GARDP” study noted that only 7.8% of patients in India with carbapenem-resistant Gram-negative bacterial infections receive the appropriate antibiotic therapy, while the rest either went untreated or it was inadequate (GARDP).
Another analysis by the Global Burden of Disease / Health Data shows that India has an attributable death count for AMR in 2021 of around 267,000 and nearly 987,000 associated deaths.
Beyond the Numbers#
The increasing rates of antimicrobial resistance have significant human, social and economic implications. Research shows that treatment failure and potentially more severe illness are the immediate human costs associated with resistance; patients suffering from infections with resistance inevitably have longer hospital stays, longer courses of antibiotics, and/ or second or third line drugs that tend to be costlier. These longer illnesses lead to greater risk of complications or even death. The cost of care rises, as resistant infections require more diagnostics, stronger and more expensive antibiotics, and intensive care, which also intensifies the financial burden to families and hospitals. At a system level, the rising costs of AMR are quite concerning. As resistant infections extend treatment or complicate an invasive life-saving medical intervention, what can be safely done in the operating room, emergency room or ambulatory diminishes when antibiotics do not provide protection when needed most. Even in larger scale, but equally significant are the macroeconomic costs; lost productivity, healthcare system pressures and financial consequences for families evidence how drug resistance is an economic issue and not just a medical problem.
What Experts Recommend#
Experts at the CIDSCON 2025 conference and healthcare partners continue to emphasize that a multifaceted approach is indispensable to end the resistome crisis in India related to antimicrobial resistance (AMR). First, we must focus on medical education by ensuring that undergraduate medical and nursing education includes strong infection prevention and control, AMR management, and stewardship. We must equip future healthcare professionals from the start. Second, we must focus on expanding diagnostics and stewardship programs. Increasing access to rapid tests involves increasing diagnostic capacity in smaller hospitals and enforcing antimicrobial stewardship programs with sufficient authority and influence to monitor prescribing. Third, we must improve community education and awareness; we need movements of people in communities to understand the harm of misusing antibiotics, avoid requiring prescriptions for antibiotics, and avoid stopping antibiotics and only use the prescribed full course of antibiotics so as not to promote resistance. Fourth, we must collect and share surveillance data showing resistance trends across urban and rural India, then create policies based on the evidence; therefore, it is very important that we have cooperative surveillance data on resistance trends across urban and rural India with appropriate institutes such as ICMR, One Health Trust and GARDP were to be the transparency leaders, which is very important and the use of urban and rural institutions for respect. Finally, we need a robust regulatory structure.
Turning the Tide#
To counter this silent invasion, India will need urgency, coordination, and sustained effort. Combating antimicrobial resistance is not a solely medical task; it’s a social necessity that costs lives, livelihoods, and our future.
India has untapped potential. The country can lead with its established pharmaceuticals sector, burgeoning diagnostic capability, and academic institutions, but action is required now:
improved diagnostics, stricter prescribing requirements, education, surveillance, and the policy will always need to be underpinned by enforcement and resources.
When managed, drug-resistant infections can be controlled, and India can reclaim its promise of public health to all citizens. Let us make this the point where awareness is transformed into action, and statistics become success stories.
With inputs from:
- Mumbai: Drug-resistant infections emerge as major public health problem in India, Times of India, Sept 2025.
- India AMR profile, HealthData.org, 2023.
- Most drug-resistant infections go untreated in India, GARDP & collaborators.
- India can lead the way in tackling antimicrobial resistance, GARDP.




Thanks for sharing. I read many of your blog posts, cool, your blog is very good. https://accounts.binance.com/register-person?ref=IXBIAFVY
Thank you for your kind words.
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.